Health
Study Reveals Potential for Expanded Donor Pool in Stem Cell Transplants

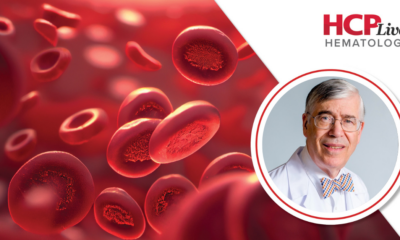
Research presented at the American Society of Hematology (ASH) annual meeting in Orlando indicates that stem cell transplants using mismatched unrelated donors (MMUDs) with less than a perfect human leukocyte antigen (HLA) match may offer similar one-year survival rates as those using better-matched donors. Specifically, patients receiving transplants with less than a 7/8 HLA match achieved a one-year survival rate of 85.6%, compared to 78.6% for those with more closely matched donor cells.
The findings suggest a significant opportunity to broaden the donor pool, which could provide hope for patients in need of transplants. The study, led by Antonio Jimenez Jimenez, MD, from the University of Miami Sylvester Comprehensive Cancer Center, also reported that rates of graft-versus-host disease (GVHD), graft failure, relapse, and non-relapse mortality were comparable between the two groups.
Significance of Expanding Donor Access
During a press briefing, Jimenez Jimenez stated, “We have shown that outcomes with less than seven out of eight grafts, using post-transplant cyclophosphamide (PTCy), appear to be comparable to 7/8 matches.” He emphasized the operational data indicating that donors are currently available, reinforcing the potential for extending donor match considerations to include all levels. This adjustment could lead to near-universal donor access, impacting patients regardless of race or ethnicity.
The importance of widening the donor base was echoed by press briefing moderator Wendy Stock, MD, from the University of Chicago. “Even though we say that we have a donor for everybody, we don’t, unless we expand the donor pool,” she remarked. Stock highlighted that the positive outcomes associated with PTCy administration are particularly encouraging, as they encourage patients to consider transplants when they are informed of their disease’s potential to recur.
Study Details and Outcomes
The findings were part of the ACCESS study, which focused on patients with hematologic malignancies requiring a hematopoietic cell transplant (HCT). The study involved patients aged 35 or younger, with a HCT comorbidity index of 0-4, who had available donor matches ranging from 4/8 to 7/8. Notably, patients with suitable 8/8 HLA-matched donors were excluded from the analysis.
The study included 278 participants, with 183 receiving 7/8 HLA matches and 85 receiving less than 7/8. The results revealed a trend towards better overall survival in the <7/8 group. Secondary outcomes at one year demonstrated that <7/8 matching had performance levels at least equal to those of 7/8 matching, including:
- GVHD-free/relapse-free survival: 53.0% vs 51.1%
– Acute GVHD grade II/IV: 34.4% vs 38.8%
– Acute GVHD grade III/IV: 7.1% vs 8.2%
– Non-relapse mortality: 8.4% vs 13.7%
Jimenez Jimenez also analyzed global registry data for 2,477 patients who had no potential 8/8 donor matches. The analysis included a demographic breakdown showing that 62.2% of these patients were ethnically diverse. He pointed out that every patient had access to multiple donors with <7/8 matching, highlighting the potential to significantly increase donor availability as the HLA match decreases. “Importantly, as we move away from seven out of eight to six out of eight, five, and four out of eight, the potential number of donors increases dramatically,” Jimenez Jimenez noted. This increase will have significant implications for patient access and equity in transplantation. While acknowledging the benefits of PTCy, Jimenez Jimenez cautioned about the associated toxicity, particularly for older patients. The ongoing OPTIMIZE trial will explore whether lower doses of PTCy can maintain transplant outcomes while reducing toxicity. Dr. Jeff Auletta, senior vice president of the National Marrow Donor Program, highlighted that about 70% of patients experienced grades II-V infections with standard PTCy, indicating a need for optimization. The trial aims to evaluate the efficacy of a 50% reduction in the typical PTCy dose on both toxicity and efficacy.
As the research unfolds, the implications for expanding donor access and improving transplant outcomes remain a critical focus in the field of hematology. The findings from the ACCESS study underscore the potential for significant advancements in patient care and accessibility in stem cell transplantation.
-

 Science2 weeks ago
Science2 weeks agoNostradamus’ 2026 Predictions: Star Death and Dark Events Loom
-
 Technology1 month ago
Technology1 month agoOpenAI to Implement Age Verification for ChatGPT by December 2025
-

 Technology6 months ago
Technology6 months agoDiscover the Top 10 Calorie Counting Apps of 2025
-

 Health4 months ago
Health4 months agoBella Hadid Shares Health Update After Treatment for Lyme Disease
-

 Health4 months ago
Health4 months agoAnalysts Project Stronger Growth for Apple’s iPhone 17 Lineup
-

 Health4 months ago
Health4 months agoErin Bates Shares Recovery Update Following Sepsis Complications
-

 Technology4 months ago
Technology4 months agoElectric Moto Influencer Surronster Arrested in Tijuana
-

 Technology5 months ago
Technology5 months agoDiscover How to Reverse Image Search Using ChatGPT Effortlessly
-
 Technology6 months ago
Technology6 months agoMeta Initiates $60B AI Data Center Expansion, Starting in Ohio
-

 Technology6 months ago
Technology6 months agoRecovering a Suspended TikTok Account: A Step-by-Step Guide
-
 Education4 months ago
Education4 months agoHarvard Secures Court Victory Over Federal Funding Cuts
-

 Technology2 months ago
Technology2 months agoDiscover 2025’s Top GPUs for Exceptional 4K Gaming Performance